This site may not work properly using older versions of Edge and Internet Explorer. You should upgrade your browser to the latest Chrome, Firefox, Edge, Safari, or any other modern browser of your choice. Click here for more information.
Your Stories
This is where we tell your stories, cover topical issues and promote meaningful initiatives.
New tool to fight infection in the tropics
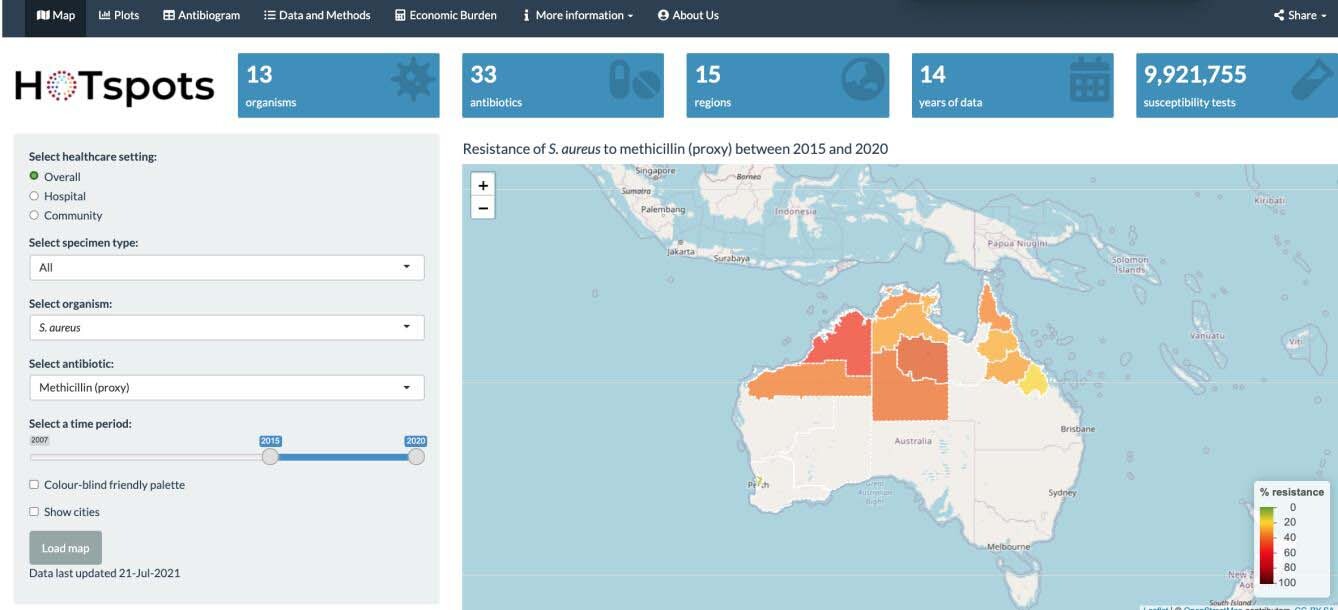
Tropical areas across the top of Australia have a very high rate of potentially dangerous skin and other infections – and a very low level of information to support clinicians in treating these patients with antibiotics. A new digital data platform aims to fill the clinical and surveillance gap – but also to “inform policy makers to invest more time and resources in regional and rural Australia”.
That’s the aim and the hope of Dr Teresa Wozniak, lead researcher of the HOTspots program which enables clinicians in northern Australia – doctors, nurses and Aboriginal health practitioners – to identify ‘the right drugs for the right bugs’.
“The platform, which provides localised and timely information about which antibiotic-resistant organisms are circulating in a given local region, will join a suite of resources to support clinicians across northern Australia to manage patients more effectively,” says Dr Wozniak, Principal Scientist at CSIRO and Honorary Senior Research Fellow at Menzies School of Health Research.
“We are constantly looking at ways to make HOTspots more user-friendly and provide local evidence so that those patients who live in resource-poor settings, despite challenges of remoteness and high turnover of healthcare staff, have equitable access to health care.”
Northern Australia, above the Tropic of Capricorn, has a low population density, with a lot of remote and regional communities, and a very high burden of infectious diseases, says Teresa. Skin infections pose a significant issue in the tropics.
“Skin is your barrier to the outside world. If that barrier is compromised, you are at a higher risk of skin infections.”
Living in remote settings further adds to that risk.
“Skin infections caused by Staphylococcus aureus (i.e golden staph) is a common one, a really big one. Other infections include urinary tract infections which, if they go untreated, can become invasive bloodstream infections.”
Dr Wozniak pointed out that a study by one of her PhD students found that clinicians in remote areas were doing a good job, wanted to do the right thing, but were hampered by a lack of resources.
“In some cases, it takes three to four days for results to come through from pathology to confirm what is causing the infection, but remote health workers don’t have time for that,” says Dr Wozniak. “The patient may be returning to their home or community and the clinician needs to make the most accurate determination on the spot and decide what treatment and antibiotics to use.
“With improved surveillance and data from the HOTspots platform, clinicians can visualise and interrogate data (by age and sex) that are relevant to the region where the patient may have acquired the infection. If he or she suspects a particular organism, they have access to information from the HOTspots platform, plus the treatment guidelines and their own expertise, to prescribe antibiotics most likely to work and kill the bacteria.”
While there have been some delays due to COVID-19, the platform is updated every six months, with plans to move towards more regular updates. HOTspots is now being used in hospitals in Northern Territory and increasingly in regional, rural and remote clinics.
The increased data collection is an important step towards the goal of health equity in Australia, says Dr Wozniak.
“With research and resources, we tend to focus on where we see the most people,” she says. “We survey the big major hospitals and tertiary hospitals and know so much about what is happening there.
“Northern Australia is geographically isolated and, in many parts, [is made up of] resource-poor settings which are often outside of surveillance reach. Until recently, this data had not been provided to treating physicians.
“We are now collecting the data, clinicians are using the data – hopefully the data will also allow some people to see the hotspots of high infections and which will need greater investment and resources.”
HOTspots was developed from funding provided by the HOT NORTH program, an NHMRC research program based at Menzies School of Health Research.
Access the platform at this link.