This site may not work properly using older versions of Edge and Internet Explorer. You should upgrade your browser to the latest Chrome, Firefox, Edge, Safari, or any other modern browser of your choice. Click here for more information.
Your Stories
This is where we tell your stories, cover topical issues and promote meaningful initiatives.
Pandemic spotlights emerging nursing workforce in the NT
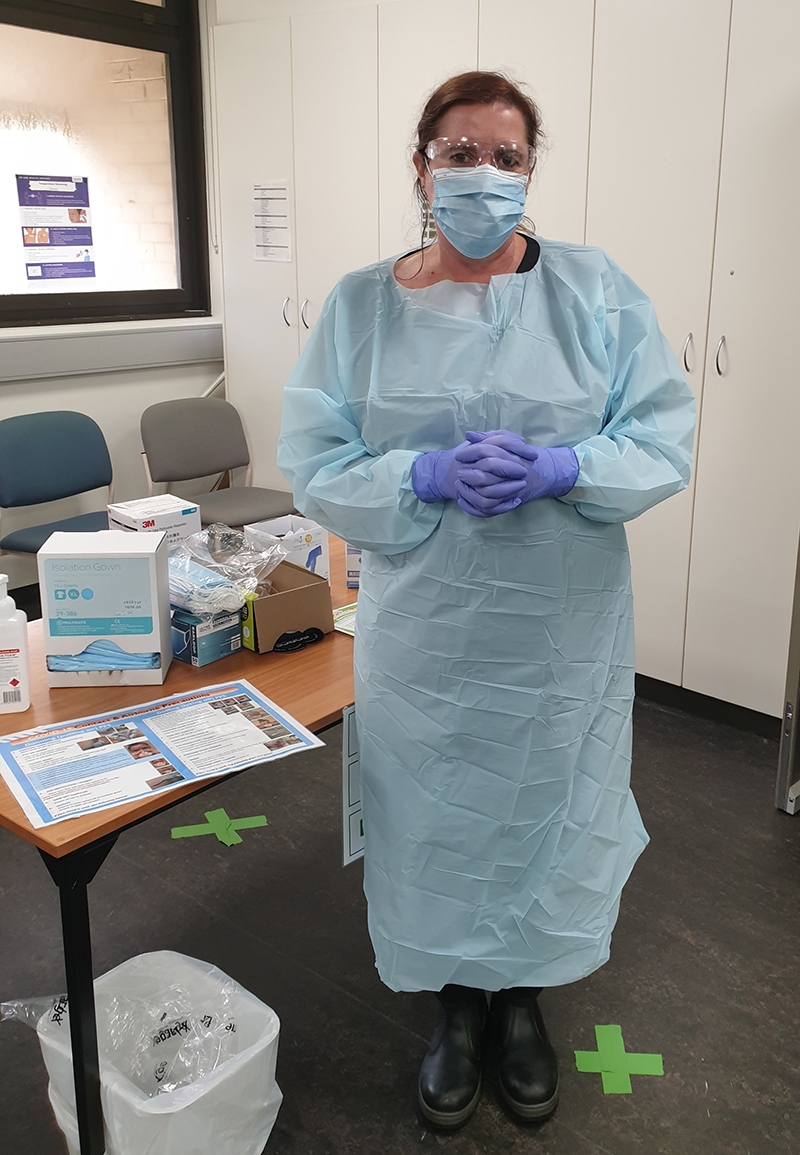
Angela Sheedy’s time at the Howard Springs quarantine facility during the pandemic has got her reflecting on the untapped skills of student and newly-qualified nurses in Australia prior to the COVID-19 pandemic. Here, she calls for an open discussion and innovation around how we implement our student and newly graduated nurses into the health workforce.
The Howard Springs quarantine centre in the Northern Territory, where 64,000 people were sent during two years of the COVID-19 pandemic, utilised student nurses and newly graduated nurses who were enlisted into the health workforce.
The junior nurses had differing knowledge bases but all had the foundations of health care. This was certainly advantageous for a quarantine facility which provided a public and primary health care overlay, according to Angela Sheedy, who was working at the facility as the Nurse Education Management Consultant.
We needed that workforce, says Angela, and now, as Senior Research Officer with Charles Darwin University’s Menzies School of Medicine, she has been tasked with exploring why the operation of the facility was so successful. She’ll be producing a report that will go towards preparing Australia for any future similar emergency.
A Registered Nurse with 20 years of practice in the NT, Angela has extensive experience working with undergraduate nursing students and a career focus on public health. She says the pandemic has put the spotlight on this source of nursing expertise and she wants to encourage an open discussion on how the health industry throughout Australia can continue to use the skills that student nurses and newly graduated nurses have learned.
“They were a terrific part of the workforce, motivated and educated,” Angela says. “We couldn’t have done what we did without the Assistants in Nursing (AINs) and new graduate and new to practice nurses.”
The facility at Howard Springs, about 30 kilometres south-east of Darwin’s CBD, once an unused workers’ camp on the city’s outskirts, was rebadged as the Centre For National Resilience. Able to house more than 2,000 people at one time, it was a temporary home for about 22,000 expat and travelling Australians, including those stranded in the centre of the pandemic in Wuhan, China, and then on repatriation flights from around the world, as well as people on humanitarian flights.
“We had to find more and more nurses, and quickly,” says Angela.
“As part of the emergency response, student nurses were implemented in the Assistance in Nursing role, a role already under consideration and fast-tracked for the COVID-19 pandemic response. In the NT, the criteria included second and third year undergraduate nursing students, and they had to have completed their first year placement, their foundations of nursing.
“Bringing in the AIN emergency workforce, we realised what an amazing untapped workforce we hadn’t used in this way before in the NT. These student nurses were very motivated and excited to be part of the pandemic response. The AINs were so very successful because we had people with health knowledge, an understanding of medical language and an understanding of the culture of a health facility all under the guidance of a senior registered nurse.
“We then turned our attention to newly graduated nurses. With the current system, new graduates may or may not get accepted immediately into the graduate nurses positions in hospitals around the country after graduation, and it may take six months or more to achieve.
“We needed this workforce and couldn’t have done what we did without the AINs and new graduate nurses. They took on core responsibilities and did a great job, which included tasks like COVID-19 health screening, COVID-19 swabbing and health assessments for any arising medical conditions.
“And previous to this many of the student nurses were working in hospitality or as orderlies or unemployed.”
Graduate nurses can register with AHPRA as soon as they finish their degree, says Angela.
“Over three years, they’ve done 800 hours of clinical practice on top of their studies,” she says. “The nurses coming out of university have current health knowledge, including the use of available technology and resources.”
Angela highlighted the industry expectation for newly graduated nurses to do another year in hospitals.
“It’s not been the Nursing or the Midwifery Board that is demanding this extra year, it’s become an expectation in acute care sectors and is considered a necessary step in a nurses’ career, by both the industry and graduate nurses.”
Hospitals receive government money for a set number of positions in a Graduate Nurse program where they are mentored and supported.
“This additional year of support is great but not every nurse gets an immediate position and it can leave newly graduated nurses in limbo,” Angela says.
“This may have no reflection on their nursing skills and knowledge but is just a result of programs being only able to offer so many positions.
“And this is in an environment where we are recognising the importance of primary care as well as specialised clinics for cancer, et cetera, keeping people out of hospitals. We are now seeing more discussion and actions to integrate these students and new nurses into these systems and benefit from their skills.”
Angela is delighted by the announcement by the NT Government to increase its graduate nurse program, to increase places in the early entry pathway for nurses and midwives with less than 12 months experience (new to practice nurses), and to increase the Assistant in Nursing (AIN) role to extend beyond acute care to include primary health care.
“This is all great outcomes for our new nurses and student nurses,” she says. “It shows the NT continues to move forwards and support this group to enter the health industry.”
Angela’s 12-month MRFF funded project with CDU will look at both the residents and the workforce, conducting surveys and looking at leadership roles.
“The workforce is a big chunk of that research,” says Angela.
“We will focus on what we did and why it worked so well. The aim is to create a toolbox to guide, what we need to do in the event of another pandemic like COVID-19.”
Read more COVID-19 content: Moral Injury and the COVID-19 Pandemic & Getting the #JabDone with Wuchopperen.