
Hi Jane,
Thanks for your question. Below, I’ve provided an overview of the approach to burns that we teach during courses, which uses the C.R.A.N.A. mnemonic.
C) Context: Your remote/isolated situation
Burn injuries pose a significant risk to the health and lives of children in Australia. Research has consistently shown that Indigenous children and those residing in rural and isolated regions bear a disproportionate burden of burn injuries – your interest in burns care is well-founded.
R) Respond: Primary Survey (+ triage considerations)
Like all traumas, paediatric burn assessments require a primary and secondary survey with the initial aim of identifying and managing immediate life threats. It’s important to not get distracted by the burn injury; a prompt and accurate initial assessment and triage are essential for ensuring appropriate and timely care. This lays the foundation for a comprehensive treatment plan.
A) Assess & Manage: Secondary Survey (+ targeted assessments & interventions)
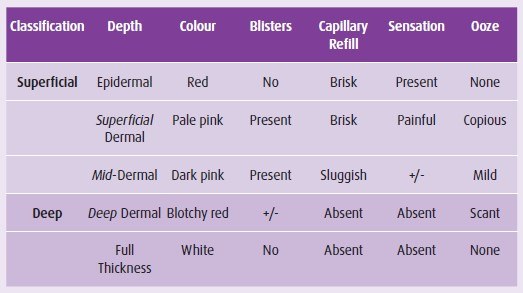
Determining burn extent and depth
An accurate assessment of burn extent and depth is crucial for determining the appropriate management strategy. In paediatric patients, this task requires careful attention due to unique anatomical and physiological considerations. Clinicians employ a combination of clinical examination, burn area estimation tools such as the Lund & Browder Chart or the Rule of 9s, and in some cases, imaging techniques to determine the precise extent and depth of the burn injury in children. Employing standardised assessment tools helps ensure consistent and reliable evaluation, enabling tailored treatment plans.
Managing Burns in Infants and Young Children
We teach the FACADE mnemonic for this step:
First aid, Analgesia, Clean, Assess, Dress, Elevate.
It’s important to note that babies and young kids have special vulnerabilities that require specific attention. Skin physiology, body surface area-to-weight ratio, and the potential for developmental complications must all be considered. Cautious fluid resuscitation, meticulous wound care, and attention to pain management are paramount. Infants and young children may be more susceptible to heat-related injuries, demanding proactive prevention strategies. A multidisciplinary approach involving paediatric specialists ensures optimal care for these young patients.
Fluid Resuscitation Guidelines
Fluid resuscitation is a critical component of managing paediatric burn patients, aiming to restore and maintain proper circulation and perfusion. However, the fluid requirements in children differ from those in adults. Careful assessment of burn size, depth, and associated factors determine the appropriate fluid resuscitation approach. The Modified Parkland Formula is the accepted standard in most clinical areas for calculating fluid requirements in paediatric burns.

N) Next step: Communication: retrieval/referral
Referring paediatric burn patients to specialised burn centres is crucial for ensuring optimal outcomes. Consider transfer when the child is requiring care beyond the comfort level of the clinic or hospital and generally for all burns that are:
- >10% TBSA
- All full thickness
- Special areas: face, ears, eyes, neck, hands, feet, genitalia, perineum, or a major joint, even if <10%
- Circumferential
- Chemical
- Electrical
- Associated with trauma and/or spinal cord injury
- All inhalation/airway
- Children <12 months
Recognising these criteria and promptly referring patients to specialised centres facilitates access to a comprehensive range of expertise, resources, and specialised therapies, ensuring the best possible care for children with severe burn injuries.
A) Assist team: Leadership in emergencies
CRANAplus encourages staff to utilise support frameworks such as the TAKE STOCK Hot Debrief Tool to ensure that you and your colleagues have an opportunity to reflect on events in a supported manner. An event meets the criteria for a hot debrief in cases of an unexpected death, distressing event, staff request, unexpected outcome, and paediatric resuscitation.
I hope this is of assistance.
Brooke Maloney
Remote Clinical Educator CRANAplus
References:
https://onlinelibrary.wiley.com/doi/full/10.1111/1753-6405.12729#azph12729-bib-0003
https://remotephcmanuals.com.au/download/39290?filename=RPHCM_STM_ Manual_8thEd.pdf
https://www.health.qld.gov.au/__data/assets/pdf_file/0016/1215043/PCCM_11th_ed.pdf
https://cdn.wchn.sa.gov.au/downloads/WCH/children/burns/paediatric-burns- assessment-form.pdf
https://www.rch.org.au/clinicalguide/guideline_index/burns/
https://www.rcemlearning.co.uk/foamed/take-stock-hot-debrief/
Assessing burn depth
