This site may not work properly using older versions of Edge and Internet Explorer. You should upgrade your browser to the latest Chrome, Firefox, Edge, Safari, or any other modern browser of your choice. Click here for more information.
Your Stories
This is where we tell your stories, cover topical issues and promote meaningful initiatives.
APSGN in focus
CRANAplus spoke with medical doctor, researcher and educator, Dr Allison Hempenstall, Public Health Medical Officer of the Torres and Cape Hospital and Health Service, to discuss the nuances of acute post-streptococcal glomerulonephritis (APSGN), its causes, symptoms,
trends and the importance of prevention strategies.
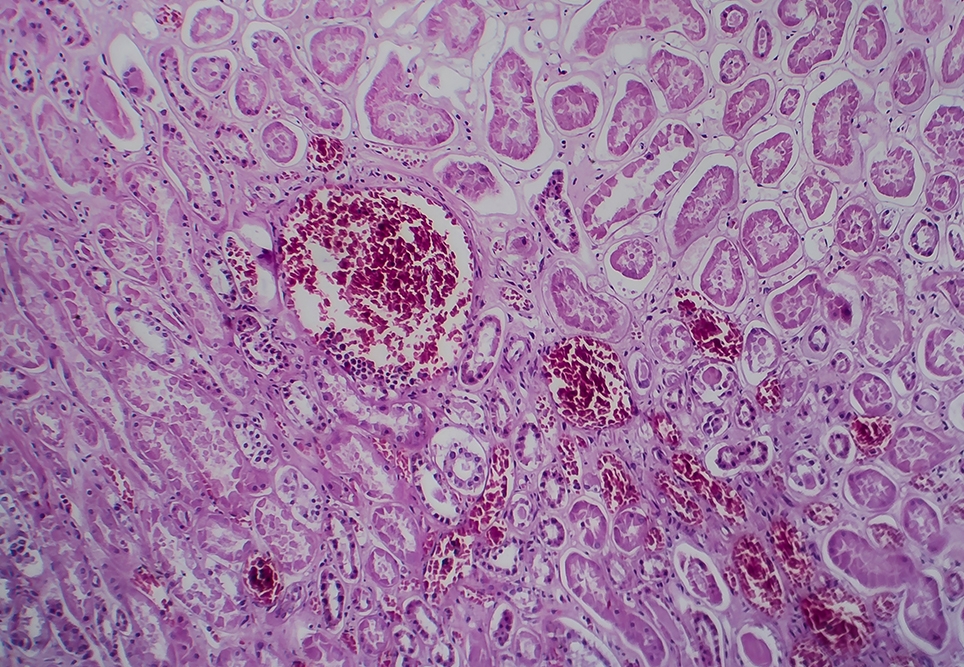
Acute post-streptococcal glomerulonephritis – otherwise known as APSGN – is an inflammatory disease of the kidneys following a skin or throat infection with Streptococcus pyogenes, known as group A streptococcus (GAS), or occasionally groups C or G streptococcus.
In Australia, reports suggest Aboriginal and/or Torres Strait Islander children have amongst the highest rates of APSGN reported worldwide, and the rate of new cases has increased over the last 25 years. Despite this, still so much is unknown about APSGNs prevalence in Australia and a lot of more can be done in the prevention of the disease.
What is APSGN and how is it caused?
APSGN stands for acute post-streptococcal glomerulonephritis. It’s an autoimmune response after exposure to a Strep A infection (e.g. tonsillitis, impetigo). Autoantibodies that are supposed to target the Strep A infection instead target the kidneys.
What is your current exposure to APSGN?
We see quite a bit of APSGN in Far North Queensland and there is emerging evidence that an episode of APSGN increases a patient’s risk of chronic kidney disease later in life. Particular virulent strains of Strep A can spread quickly through a community and cause an APSGN outbreak. All these things are important to understand better in order to try and reduce and ultimately prevent cases.
What are the common symptoms and complications associated with APSGN?
The symptoms include: oedema (facial or peripheral), hypertension and haematuria. Complications range from hypertensive crisis
(acute) through to chronic kidney disease (chronic).
What trends have you observed in the incidence of APSGN in Australia over recent years?
We know that there are higher rates of APSGN in First Nations communities, especially those who are socio-economically disadvantaged, as this essentially is a disease of socio-economic disadvantage. But overall, I don’t think we really have a good grasp on the true incidence of APSGN in Australia. I would hope that as socio-economic disadvantage improves over time, APSGN cases will decline.
How does the prevalence of APSGN in First Nations communities compare to other populations in Australia?
Although the evidence is limited, some studies have reported that the prevalence of APSGN in First Nations communities is higher than non-First Nations communities.
What are the major challenges in addressing APSGN outbreaks in remote communities?
There are many challenges including access to remote locations (especially in the wet season when transport may be limited) and human resources (outbreak responses are resource intensive and often require a team to fly into a community and work in partnership with the local staff).
What preventative measures can communities take to reduce the incidence of APSGN?
Have you heard of the nine healthy living practices? These are: washing people, washing clothes and bedding, removing wastewater, improving nutrition, reducing overcrowding, reducing insect bites, reducing impacts of dust, controlling the temperature of the living environment, reducing hazards that cause trauma.
How effective are current treatment options for APSGN, and what is the prognosis for affected individuals?
Current treatments for APSGN include stopping the Strep A with a long acting penicillin antibiotic; managing high blood pressure with antihypertensives; and managing oedema.
What policy changes would you advocate for to improve the management and prevention of APSGN in Australia?
Healthy housing is a human right. Yet in Australia – many people of all ethnicities do not live in safe and healthy housing. This is everybody’s issue that we must address at a local, state and national level.
How can healthcare systems better engage with First Nations communities to address health disparities related to APSGN?
Ensuring any local public health responses are First Nations-led and in close partnership with local First Nations communities (for example the local council and local healthcare centre).
What do you see as the future directions for research and public health policy regarding APSGN?
We need to better understand APSGN across all of Australia. There has been fantastic epidemiological research from the Northern Territory, however we need to understand the disease in other areas such as Queensland.
Are there any promising develop-ments, such as potential vaccines or innovative treatment strategies, on the horizon for APSGN?
The Australian Strep A Vaccine Initiative (ASAVI) is an Australian-led global initiative with the goal of reducing the disease burden caused by Group A Streptococcus (Strep A) infection through effective vaccination.
References
For more information on Healthy Living Practices, visit: https://www.health.nsw.gov. au/environment/aboriginal/Pages/healthy-living-practices.aspx