Strongyloidiasis often evades detection, with dangerous consequences. What about the disease makes it easy to miss?
Strongyloidiasis doesn’t necessarily have specific symptoms, and because Strongyloides stercoralis is microscopic, you won’t see it.
Being aware is vital, and having it in mindas a differential diagnosis. My journey began by looking first at the unwell patient – with septicaemia or meningitis – and asking why would a 25-year-old male be at risk of dying from septicaemia?
What’s the connection between septicaemia and strongyloidiasis?
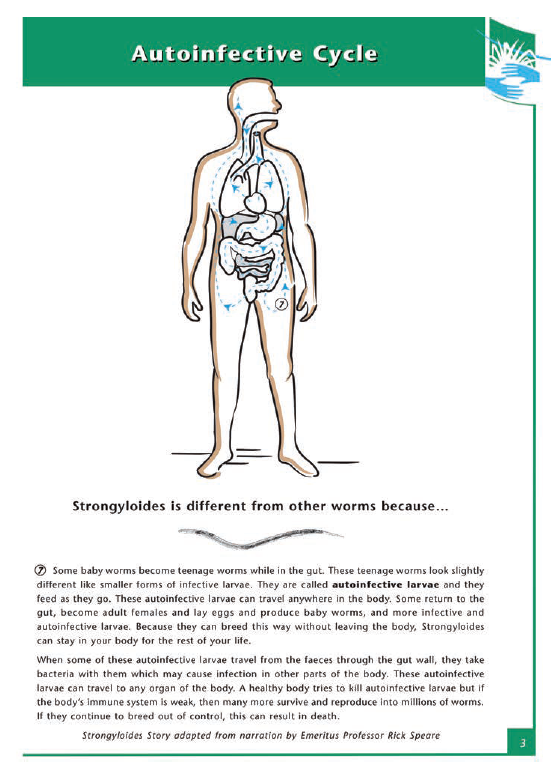
With strongyloidiasis, autoinfective filariform larvae can travel from the bowel and burrow through the gut lining.
When they do this, they can also take with them bacteria from the bowel to any organ of the body. That’s where septicaemia and other bacterial diseases can come in.
Disseminated strongyloidiasis, the most advanced phase of the disease, can also increase the risk of multiple-end organ failure and has a high fatality rate. What precipitates it?
People who are immunosuppressed are at the greatest risk. In one study 65% of the fatalities from disseminated strongyloidiasis were associated with giving corticosteroids. The thinking is that it has a dysregulation effect. I see Strongyloides stercoralis in a David Attenborough way. It’s a survival mechanism. When the parasite senses that its home in the human is no longer safe, it says, “I need to find another home.” It starts multiplying into its millions, and the infection becomes out of control.
What advice can nurses give, and follow, when it comes to preventing infection?
Patients want to know about Strongyloides, what it is, where it lives, what makes it special, how it affects the body, how it can be diagnosed and treated, and how they can prevent it.
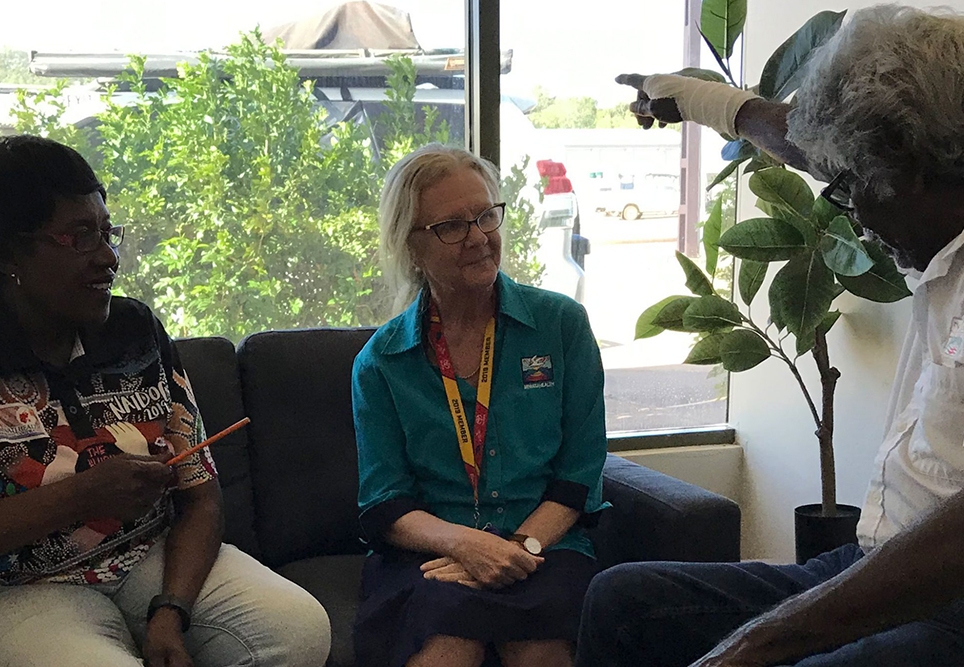
We developed the Strongyloides patient education flip chart in early 2002 and it is a very useful visual aid. It’s available on the strongyaust.au website.
Strongyloides stercoralis survival outside the body is limited. It looks for a warm host and enters through the skin. Wearing shoes makes a difference – if you’re in an area where there is potential for faecal contamination. If you’re handling faeces at any point of time, that’s potentially infectious.
Persons with disseminated strongyloidiasis are also infectious with cases diagnosed from sputum or skin. Everyone will do their best to prevent it, but I am aware of clinicians who have become infected.
How about primordial prevention?
We see One Health as a way to address strongyloidiasis. One Health considers humans as well as animal health and environmental health. At the environmental level, transmission happens when there’s inadequate access to clean water and sanitation – a basic human right and United Nations Sustainable Development Goal Number 6.
We see having strongyloidiasis made notifiable as a way to identify hotspots. The World Health Organisation (WHO) has also now included strongyloidiasis within the neglected tropical diseases for elimination by 2030.
Do you think that can be done?
Australia needs to start acting. Dismissive comments like “why bother to treat the asymptomatic” or “they’ll only get it again” have always upset me. Australia could be leading the way in how we address this – because we can do something, just like Miwatj has. We need to look at this as a chronic infectious disease that is treatable and curable if diagnosed early.
The systematic approach of including strongyloidiasis in a preventative health assessment is vital for all endemically infected communities in Australia. Otherwise, controlling this disease is dependent on individuals, and individuals come and go.
Control programs in endemic communities are feasible – your work has produced reductions as dramatic as 60 to 10 per cent prevalence.
10 per cent is certainly a reduction, but still 10 times what you would expect in a suburb of Brisbane. My focus is on closing that gap.
By identifying strongyloidiasis, we’re also identifying the communities that are at the greatest risk for other diseases, and in greatest need of further infrastructure – for example, housing and sanitation facilities. It’s a proxy for reducing other conditions you don’t expect to have in Australia.
Your passion is inspiring. What has motivated you to take on strongyloidiasis and what has kept you going?
My strongyloidiasis journey began in 1995, with a parasitology course and Rick Speare being a fantastic mentor. Cases of disseminated strongyloidiasis were unfolding around this time, then in 1999, my colleague, friend and mentor, an Aboriginal Health Worker who was a queen for her people, developed a condition and went to Darwin. Instead of being able to come back and have that managed at home, she died in Adelaide from disseminated strongyloidiasis. It was a huge loss. It becomes personal when it is someone you know.
In 2000 we introduced ivermectin, which made a big difference. When I was speaking to her sister and explaining what we were doing, she said to me, “let not her death be in vain”.
When you’re the community doctor, you learn about what is relevant in your community. There were times I could have walked away, but I felt I had been given this responsibility to take further forward. And I wasn’t on my own.


What can health professionals do to limit the risk of disseminated strongyloidiasis?
Health professionals working in community primary healthcare services understand the value of early diagnosis, treatment and follow-up testing, and are best placed to prevent clinical complications for strongyloidiasis.
The CARPA manual recommends that anyone who is going to be immunosuppressed needs to be tested for strongyloidiasis; but if they’re coming from a known endemic area, they also need to be given ivermectin treatment before they start their immunosuppressants.
The best way of finding and treating people before they develop severe clinical complications is in the chronic phase and the best test for that is Strongyloides serology, though it may not detect newly acquired or disseminated cases. This can be included with the adult health check/preventative health assessment along with STIs, hepatitis B, diabetes, and chronic kidney disease. Follow up serology 6 to 12 months after treatment is recommended as serology decreases to negative with effective treatment. Some cases may require repeat treatment for eradication.
Ivermectin should be given to all positive cases. We started using ivermectin in 2000 because it was more effective for strongyloidiasis.
Before that I remember albendazole being introduced in 1995. That made a huge difference to a number of other helminths. But for S. stercoralis, it’s not enough to reduce the worm load – you need to eradicate each last worm due to its auto-infective cycle.
International guidelines in the 1990s recommended treating all infected persons, including the asymptomatic, as life threatening complications are unpredictable.
Strongyloides serology has been included in the Refugee Health Assessment since 2010 and those with positive and equivocal results are treated to prevent clinical complications and transmission.
By treating the people that test positive, you’re also preventing transmission, because it’s humans that will take it from one place to another – hence desert communities can have Strongyloides as well. It is not something that relates just to the tropics.
